Have you ever tried looking for a samoyed in the snow? What about one that couldn't bark and was the size of a chihuahua?
That's what mammogram technology has been working with – tumors appear like small white masses on white backgrounds in the denseness of breast tissue.
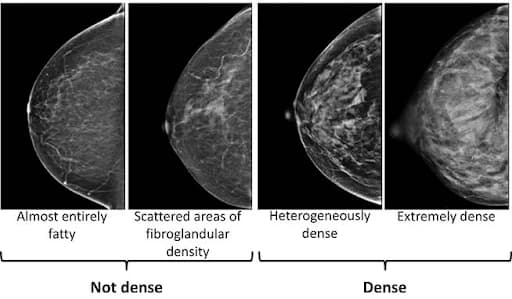
Image via Fred Hutchinson Cancer Center
Studies show that dense breast tissue can reduce the accuracy of mammograms by 40-50%. In other words, nearly half of cancers may be hidden on the very test most women depend on.
This is especially important because younger women are more likely to have dense breast tissue – and that's exactly when mammography is most likely to miss something.
Ranking Breast Cancer Screening Technologies
Not all breast imaging is created equal.
S-Tier: Dedicated Breast MRI with Contrast
Breast MRI isn't just good – it's the most sensitive breast imaging tool available today.
Unlike mammography, MRI performance isn't affected by breast density. Dense tissue can hide cancers on a mammogram because both appear white on X-ray. But MRI works differently — it uses contrast to highlight blood flow into suspicious lesions, making tumors visible regardless of tissue density. That's why MRI consistently outperforms mammography in women with dense breasts.
Multiple large studies report 94.7–97.3% sensitivity for MRI in dense breasts – the highest detection rate of any imaging modality (PMC 2025; PMC 2024).
When added to mammography for women with dense breasts, breast MRI finds 16–17 more cancers per 1,000 screenings — roughly three times more than mammography alone. On follow-up annual MRIs, it detects an additional 6–7 cancers per 1,000 exams.
So why isn't MRI offered to everyone?
Despite being more accurate, breast MRI is still not the standard of care for average-risk women. Current guidelines reserve it for women with a 20% or greater lifetime risk, mostly due to concerns about cost and accessibility. For high-risk women, MRI screening is already proven to be cost-effective, and its value increases as risk increases. But for average-risk women, cost has historically been the main argument against using MRI on a broader scale.
A recent study challenges that assumption.
In a simulation of 2.5 million average-risk women, baseline MRI screening cost $1.6 billion, compared to $0.54 billion for mammography.
But over time, the economics flipped.
By year 24, the total cost of MRI and mammography programs was almost identical ($13.02B vs. $13.03B). And when the model used a more realistic MRI price based on Medicare rates ($400 per exam instead of $549), the shift happened even faster:
- MRI became more cost-effective than mammography in less than 6 years ($3.41B vs. $3.65B)
- By year 12, the total cost was 22% lower
- By year 30, the total cost was 38% lower
In other words: MRI starts out more expensive, but over time, it actually saves money.
Who benefits the most from breast MRI?
- Women with BRCA1/2, TP53, PALB2, ATM, CHEK2, or other genetic mutations
- Women with very dense breast tissue, where mammograms miss cancers
- Patients needing cancer staging or pre-surgical planning
- Monitoring treatment response, especially during chemotherapy
- When mammography or ultrasound is inconclusive but suspicion remains high
A-Tier: Contrast-Enhanced Mammography (CEM)
A strong alternative when MRI is unavailable. The scan uses iodine contrast and dual-energy mammography to highlight blood flow to tumors. Sensitivity is high (89–97.7%), making it far more effective than standard mammography in dense breasts – but slightly less sensitive than MRI overall.
A contrast-enhanced mammogram (CEM) is just like a regular mammogram, but with an additional step. Before receiving a mammogram, you get an IV injection of iodine-based dye.

On the left is a standard 2D mammogram – the breast tissue appears dense, and the cancer is barely visible (indicated by the arrowhead). On the right is a contrast-enhanced mammogram of the same breast, which clearly outlines the cancer's size and shape and confirms it's the only tumor present (arrow).
Photo Courtesy of MD Anderson
The limitations:
Like all contrast-based imaging, CEM isn't perfect. It works by highlighting areas with increased blood flow, so cancers that don't produce strong contrast uptake can remain difficult to detect. This includes some invasive lobular carcinomas, which tend to grow in a more diffuse pattern, and pure microcalcifications, which may indicate early ductal carcinoma in situ (DCIS) but don't enhance well with iodine contrast. CEM is also slightly less sensitive than breast MRI when both are tested head-to-head, meaning MRI will detect a few cancers that CEM might miss — especially in high-risk women or those with very aggressive tumor types.
There are also practical limitations:
- CEM involves radiation exposure (similar to or slightly higher than a standard mammogram)
- Requires IV contrast, which carries a small risk of allergic reactions or kidney strain in vulnerable patients
- It currently has no standardized national screening guidelines, so its use varies by facility and physician preference
Who benefits most:
CEM is particularly useful for women with dense breast tissue who need better detection than standard mammograms can provide – but who can't access, tolerate, or afford MRI. It's faster, more widely available, less expensive than MRI, and uses the same equipment and positioning as a traditional mammogram, making it easier to adopt into routine care.
It's FDA-approved for diagnostic evaluation, such as when a mammogram or ultrasound shows something suspicious, and it's increasingly being used for supplemental screening, especially in women with intermediate risk (e.g., a family history or prior atypia but not BRCA-level risk). Some centers also use it for monitoring response to chemotherapy, evaluating extent of disease before surgery, or as an option for claustrophobic or pacemaker patients who can't undergo MRI.
B-Tier: Digital Breast Tomosynthesis (3D Mammography)
This is the upgrade most screening centers have implemented over the past decade. Instead of two flat images, digital breast tomosynthesis (DBT or 3D mammography) takes multiple images from different angles and reconstructs them into a 3D view.
3D mammography detects 5.3 cancers per 1,000 screenings, compared to 4.5 per 1,000 with standard 2D mammography (Yale Cancer Center, 2024; Breastcancer.org, 2023). That's an additional 1.6 cancers per 1,000 women screened (PMC, 2021).
DBT also reduces false positives – 7.2% with DBT vs. 10.6% with 2D mammography (Yale Cancer Center, 2024). That means fewer women are called back unnecessarily for extra imaging, biopsies, and the stress that comes with them.
The downside: Cost.
3D mammography (DBT) costs about $56–$108 more per screening than standard 2D mammography, and not all insurance plans cover the difference. Still, it's becoming widely available — as of 2023, about 85% of U.S. screening centers offer DBT.
Who benefits most:
Pretty much everyone. Research shows that 3D mammography improves cancer detection and reduces false positives across all age groups and breast density levels. The benefit is noticeable in all women but is most statistically significant in those with less dense breast tissue.
C-Tier: Standard 2D Digital Mammography
This is what most people think of when they hear "mammogram." Each breast is compressed and imaged from two angles using low-dose X-rays.
Mammography detects about 4–4.5 cancers per 1,000 screenings (American Cancer Society, 2024). But that number hides something important — sensitivity changes depending on age, breast density, and hormone use.
Here's what the data shows:
| Group | Sensitivity (Cancer Detection Ability) |
|---|---|
| Women <40 | 54% |
| Age 40-49 | 77% |
| Age 50-64 | 78% |
| Age >64 | 81% |
Mammography works best in older women with non-dense breast tissue. It struggles the most in younger women and those with dense breasts.
Why it still matters
Mammography has been shown in randomized clinical trials to reduce breast cancer mortality. It's accessible, covered by insurance under the Affordable Care Act with no co-payment, and widely available.
Who benefits most
- Women 50 and older with non-dense breasts
- Women in rural or underserved areas without access to advanced imaging
- Those needing routine annual screening without high genetic risk
- Patients who cannot afford or tolerate MRI or CEM
How Does Full-Body MRI Stack Up?
Unlike a dedicated breast MRI, full-body MRI is typically done without contrast and without specialized breast coils. In breast MRI, the patient lies face down in a coil designed to surround each breast and maximize signal, detail, and contrast uptake. In full-body MRI, the patient lies on their back, and the scanner uses general-purpose coils, which means breast tissue is positioned differently and image resolution is lower.
Because of that, there haven't been large clinical trials proving that non-contrast full-body MRI can reliably detect early breast cancers the way dedicated breast MRI can. It can still identify many breast lesions – even small ones – and it may be a useful supplemental tool, particularly for people already undergoing whole-body screening for other reasons.
However, professional radiology societies currently do not recommend full-body MRI as a replacement for routine mammography or dedicated breast MRI in women at high risk. It works best as a complement, not a substitute.
Age, Demographics, and What Actually Matters for You
Screening isn't one-size-fits-all. Your age, breast density, family history, and access all shape what screening makes sense.
Screening Guidelines for Average-Risk Women (Age 40–80)
Start annual mammograms at age 40.
Why age 40?
- Breast cancer rates increase beginning in the early 40s.
- 1 in 6 breast cancers occur in women in their 40s.
- Annual screening detects cancers earlier and saves more lives than waiting until 50 or screening every two years.
What about USPSTF saying every two years?
That recommendation is designed for population-level, cost-effective policy, not for maximizing early detection. The ACR, NCCN, ACS, and ACOG all support starting at 40 – preferably annually.
What If I Have Dense Breasts? (40-50% of Population)
Dense breast tissue makes cancer harder to detect on mammograms and increases risk.
- You should still get a mammogram every year.
- Ask your doctor if supplemental screening makes sense:
- ▸ 3D Mammography / DBT (better than 2D for dense breasts)
- ▸ Contrast-Enhanced Mammography (CEM)
- ▸ Breast MRI (most sensitive option – especially useful if you also have risk factors)
What If I'm High-Risk (Genes or Strong Family History)?
This is where screening changes.
You're considered high-risk if you have:
- BRCA1, BRCA2, PALB2, TP53, ATM, CHEK2, etc.
- A strong family history of breast or ovarian cancer
- Prior chest radiation (e.g., for Hodgkin's lymphoma)
For these women:
- Start annual breast MRI at age 25–30
- Add annual mammograms by age 30
- Some alternate MRI and mammogram every 6 months
So, Is Mammography Outdated?
Not exactly. But on its own, it's no longer enough.
2D mammography is outdated for most women.
3D mammography (DBT) should now be considered the baseline standard – it detects more cancers and causes fewer false alarms than 2D.
But for many women, especially those with dense breast tissue or elevated risk, even 3D mammography isn't sufficient on its own.
- Breast MRI with contrast is the most sensitive screening test we have – nothing detects more cancers earlier.
- Contrast-Enhanced Mammography (CEM) sits in between MRI and mammography – more sensitive than 3D mammography, more accessible than MRI.
So the real question isn't "Is mammography outdated?"
It's this: Are you getting the right screening for your risk, your breast density, and your age?
What You Should Do About It
- Know your breast density. Your mammogram report should include this. If it doesn't, ask. Many states require notification by law.
- Ask what technology your facility uses. Is it 2D or 3D? Do they offer CEM? Is breast MRI available if you need supplemental screening?
- Understand your risk. Family history matters. Genetic testing matters. If you're at elevated risk, standard screening guidelines don't apply to you.
- Don't let cost perception stop you. Free and low-cost mammography programs exist through the CDC's National Breast and Cervical Cancer Early Detection Program and other initiatives (CDC, 2024). The actual cost is often lower than people think.
The Bottom Line
Don't discount mammography just yet. But the conversation about breast cancer screening is changing faster than most people realize. Technology has evolved. Guidelines have expanded. And the gap between what's possible and what's accessible has never been wider.
If you're still getting 2D mammograms when 3D is available, you're using outdated technology. If you have dense breasts or high genetic risk and no one has discussed supplemental screening, you're underscreened.
Screening saves lives. But only if it's the right screening, at the right time, with the right technology. And that's a conversation worth having with your doctor – this year, not next November.
Note: Always discuss screening plans with your healthcare provider. These are general guidelines, not medical advice.
References
[1] American Cancer Society. (2024). Breast cancer facts & figures 2024-2025. link
[2] American College of Obstetricians and Gynecologists. (2013). Management of women with dense breasts diagnosed by mammography. Committee Opinion, 625. link
[3] American College of Obstetricians and Gynecologists. (2024, October 16). ACOG updates recommendation on when to begin breast cancer screening mammography. link
[4] American Society of Clinical Oncology. (2024, September 30). Racial disparities and strategies for improving equity in diagnostic breast imaging. link
[5] ARA Health Specialists. (2023, March 14). Enhancing breast health with contrast-enhanced mammography. link
[6] Biograph. (2025, June 4). Whole-body MRI for early disease detection. link
[7] BMJ Open. (2025, January 31). National yearly cost of breast cancer screening in the USA and estimated costs by age and breast density. link
[8] Breastcancer.org. (2023, May 24). Huge study shows 3D mammograms better than 2D. link
[9] Breastcancer.org. (2024, July 17). Breast MRI: What it is, why it's done, & more. link
[10] Breastcancer.org. (2025, September 30). Mammogram screening guidelines 2025: How often to get one? link
[11] Centers for Disease Control and Prevention. (2024, April 8). Cost and access are not the only barriers women face in getting lifesaving mammograms. link
[12] Clinical Advisor. (2025, June 15). Latest recommendations for breast cancer screening & diagnosis. link
[13] DenseBreast-info, Inc. (2023, August 7). Contrast-enhanced mammography (CEM). link
[14] Mango, V. L., Goel, A., Mema, E., et al. (2019). Breast MRI screening for average-risk women: A Monte Carlo simulation cost-benefit analysis. Journal of Magnetic Resonance Imaging, 49(7), e216–e221. link
[15] Memorial Sloan Kettering Cancer Center. (2025, June 3). CT scan vs. MRI: What's the difference? link
[16] National Cancer Institute. (2023, March 2). BRCA1 and BRCA2: Cancer risks and management (PDQ®). link
[17] PMC (National Institutes of Health). (2006). Cost as a barrier to screening mammography among underserved women. link
[18] PMC (National Institutes of Health). (2009, January 12). Cost-effectiveness of MRI compared to mammography for breast cancer screening in a high risk population. link
[19] PMC (National Institutes of Health). (2018, December 5). Whole-body magnetic resonance imaging for the assessment of patients with breast cancer. link
[20] PMC (National Institutes of Health). (2019, January 10). Breast MRI screening for average-risk women: A Monte Carlo simulation cost-effectiveness analysis. link
[21] PMC (National Institutes of Health). (2020, October 24). Pros and cons for breast cancer screening with tomosynthesis. link
[22] PMC (National Institutes of Health). (2021, May 19). Accuracy of digital breast tomosynthesis for detecting breast cancer. link
[23] PMC (National Institutes of Health). (2023, May 26). Panoramic magnetic resonance imaging of the breast with a wearable coil. link
[24] PMC (National Institutes of Health). (2024, May 14). Comparison of the effectiveness of contrast-enhanced mammography recombinant images in extremely dense breasts versus the all-densities population. link
[25] PMC (National Institutes of Health). (2025, January 10). Accuracy of abbreviated breast MRI in diagnosing breast cancer in women with dense breast tissue. link
[26] PMC (National Institutes of Health). (2025, February 16). National yearly cost of breast cancer screening in the USA and estimated costs by age and breast density. link
[27] Radiological Society of North America. (2023, August 14). Comparative performance of contrast-enhanced mammography and abbreviated breast MRI for breast cancer screening. Radiology, 308(3). link
[28] Radiological Society of North America. (2025, June 1). MRI for dense breasts: Weighing the benefits. link
[29] Radiological Society of North America. (2025, October 19). Contrast-enhanced mammography as an alternative to MRI for breast cancer screening. link
[30] Radiologyinfo.org. (2024, September 17). Breast MRI. link
[31] Society of Breast Imaging. (2023, April 11). Contrast enhanced digital mammography. link
[32] Susan G. Komen Foundation. (2025, June 3). Comparing breast cancer screening rates among different groups in the U.S. link
[33] The Lancet. (2025, May 20). Comparison of supplemental breast cancer imaging techniques in women with dense breasts: A randomised clinical trial. The Lancet, 405(10389), 2123-2134. link
[34] Translational Breast Cancer Research. (2025, April 29). Contrast-enhanced mammography in high-dense breasts: A paradigm shift. link
[35] U.S. Preventive Services Task Force. (2024, April 29). Breast cancer: Screening. link
[36] Yale Cancer Center. (2024, September 16). Advanced 3D mammography detects more breast cancers, fewer false positives. link